Prediabetes, a condition characterized by elevated blood sugar levels that are not yet high enough to be classified as diabetes, affects millions globally. As the understanding of this condition deepens, new medications are emerging to help manage it more effectively. This article delves into the top prediabetes medications of 2024, exploring the latest FDA-approved treatments, comparing traditional and newer options, and discussing potential side effects. By integrating these medications with lifestyle changes, individuals can optimize their blood sugar management. We also look ahead to the future of prediabetes treatment, highlighting promising emerging therapies and breakthrough developments.
nozaviral.com offers a detailed exploration of this topic.
1. Overview of the Most Commonly Prescribed Prediabetes Medications in 2024
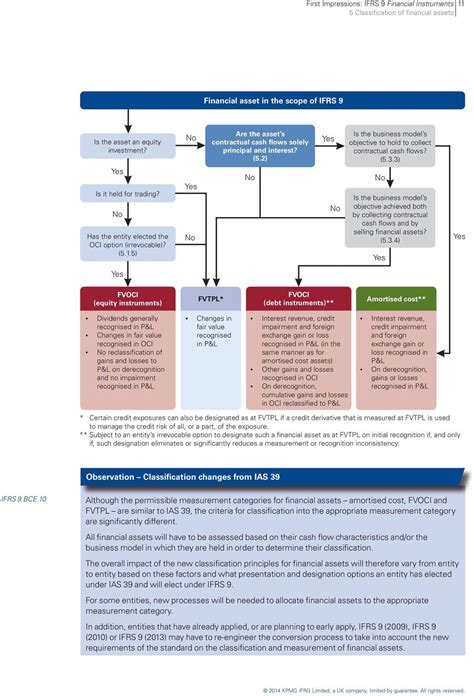
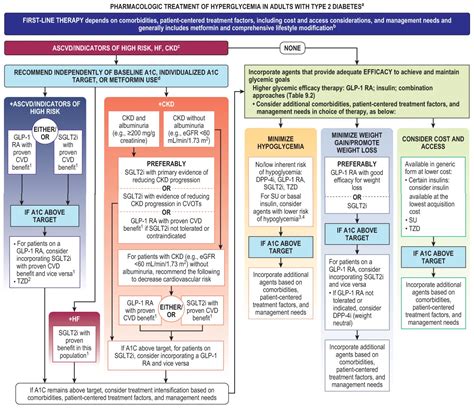
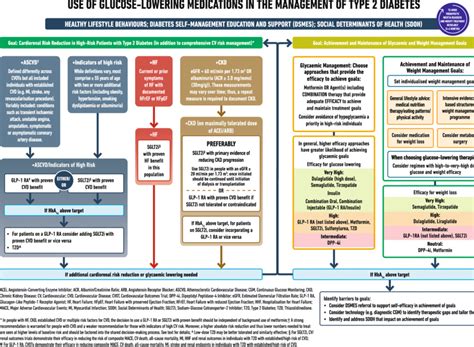
Managing prediabetes with medication has become a crucial strategy in 2024 for individuals aiming to prevent type 2 diabetes. Multiple medications are frequently prescribed to regulate blood sugar levels in those diagnosed with prediabetes. Metformin remains a fundamental treatment, renowned for its efficacy in lowering glucose production in the liver and enhancing insulin sensitivity. Other medications, such as GLP-1 receptor agonists, have gained widespread acceptance due to their dual function of controlling blood sugar and promoting weight loss, which is often advantageous for prediabetic patients.
SGLT2 inhibitors are another class of medications gaining popularity in prescriptions. These drugs work by enhancing the kidneys’ ability to remove excess glucose through urine, consequently lowering blood sugar levels. Furthermore, DPP-4 inhibitors may be prescribed for some patients, as they function by extending the activity of hormones that stimulate insulin release. Each of these medications has undergone extensive research and is commonly prescribed based on individual patient needs, allowing for a personalized approach to managing prediabetes effectively.
2. Latest FDA-Approved Medications for Prediabetes and Their Benefits
In 2024, the FDA has granted approval to several novel medications for prediabetes, expanding treatment options for patients. These medications represent breakthroughs in diabetes prevention and treatment, utilizing innovative approaches to address the root causes of elevated blood sugar. A particularly noteworthy approval is Tirzepatide, a dual GIP and GLP-1 receptor agonist, which has demonstrated impressive efficacy in reducing blood glucose levels and facilitating substantial weight loss. This medication is particularly advantageous for individuals grappling with obesity, a prevalent risk factor for the progression from prediabetes to type 2 diabetes.
Imeglimin, a newly approved drug, is a novel compound that targets mitochondrial dysfunction. Mitochondrial dysfunction is believed to contribute significantly to the development of insulin resistance. Imeglimin’s unique mechanism of action complements existing therapies, providing healthcare providers with an additional tool for creating personalized treatment plans.
Newly FDA-approved medications offer a comprehensive approach to prediabetes management. Beyond improving blood sugar control, they effectively address weight management and enhance insulin sensitivity, making them valuable tools in the fight against this serious condition.
3. Comparing Traditional vs. Newer Medications for Blood Sugar Management
The treatment landscape for prediabetes has evolved in 2024, presenting patients with a range of both traditional and newer medications for blood sugar management. Traditional options like Metformin remain a popular choice due to their established efficacy in reducing glucose production and enhancing insulin sensitivity. Metformin’s affordability and limited side effects have cemented its position as a cornerstone of prediabetes care.
While traditional medications focus primarily on glucose control, newer drugs like GLP-1 receptor agonists and SGLT2 inhibitors offer additional advantages. GLP-1 receptor agonists not only reduce blood sugar but also promote weight loss, a crucial aspect of prediabetes management. SGLT2 inhibitors, on the other hand, work by increasing glucose excretion through urine, thereby lessening the strain on insulin production and contributing to effective blood sugar regulation.
Traditional medications effectively manage prediabetes, but newer drugs offer additional advantages by addressing the broader metabolic issues associated with the condition. Selecting the appropriate treatment often hinges on individual patient needs, with some patients potentially benefiting more from the comprehensive approach provided by newer medications.
4. Potential Side Effects and Risks Associated with Prediabetes Medications
Prediabetes medications are essential for managing blood sugar and preventing type 2 diabetes, but they can have potential side effects and risks. Although medications like Metformin are generally well-tolerated, they may cause gastrointestinal problems such as nausea, diarrhea, and stomach discomfort, particularly when initially starting treatment. Furthermore, long-term use of Metformin could lead to a risk of vitamin B12 deficiency.
Newer medications, such as GLP-1 receptor agonists, may lead to side effects like nausea, vomiting, and, in some cases, pancreatitis. SGLT2 inhibitors, while effective, carry risks including urinary tract infections and an increased likelihood of dehydration due to their mechanism of action.
Tirzepatide, a newer option for prediabetes management, can sometimes lead to gastrointestinal issues. While animal studies have linked it to a potential risk of thyroid tumors, the significance for humans remains unclear. Patients should discuss these potential risks and benefits with their healthcare provider before starting treatment.
5. Integrating Medications with Lifestyle Changes for Optimal Results
Managing prediabetes effectively requires a combined approach of medication and lifestyle modifications. While medications such as Metformin, GLP-1 receptor agonists, and SGLT2 inhibitors can significantly reduce blood sugar levels, their impact is maximized when integrated with a healthy lifestyle. Diet and exercise are crucial components, enhancing the efficacy of these medications. A balanced diet featuring whole grains, lean proteins, and vegetables helps regulate blood sugar levels. Simultaneously, regular physical activity improves insulin sensitivity and aids in weight loss, further contributing to overall prediabetes management.
Lifestyle modifications play a crucial role in complementing medication effectiveness. They can reduce the necessary dosage or even eliminate the need for medication entirely. For instance, shedding 5-7% of body weight can substantially diminish the risk of developing type 2 diabetes from prediabetes, further amplifying the benefits of drug treatment.
Managing stress and getting enough sleep are also essential. Chronic stress and poor sleep habits can negatively affect blood sugar control, diminishing the positive effects of medication. Therefore, a comprehensive approach encompassing medication, diet, exercise, and stress reduction is vital for achieving the most favorable results in prediabetes management.
6. Future Directions in Prediabetes Treatment and Emerging Medications
The future of prediabetes treatment holds exciting prospects, fueled by groundbreaking medications and cutting-edge strategies. A particularly promising avenue of exploration is personalized medicine. This approach customizes treatment plans based on an individual’s genetic profile, lifestyle choices, and specific health concerns. By tailoring interventions to each patient’s unique characteristics, personalized medicine has the potential to enhance treatment effectiveness while minimizing adverse effects.
Emerging medications are increasingly focused on addressing the underlying causes of insulin resistance and impaired glucose tolerance. Drugs targeting mitochondrial function, such as Imeglimin, represent a new wave in prediabetes treatment, offering unique mechanisms of action beyond traditional glucose-lowering therapies. Furthermore, the development of combination therapies, which utilize multiple drugs to target different aspects of glucose metabolism, holds the potential for more comprehensive management of prediabetes.
In addition, technological advancements, including continuous glucose monitors and digital health tools, are expected to be instrumental in the future of prediabetes care. These tools facilitate real-time monitoring and data-driven modifications to treatment plans, resulting in more precise and responsive management. As research continues to advance, the next decade may witness further breakthroughs, revolutionizing the way prediabetes is treated and ultimately lessening the global burden of diabetes.
In summary, managing prediabetes in 2024 involves a range of medications from traditional options like Metformin to innovative treatments such as GLP-1 receptor agonists and Imeglimin. Combining these medications with lifestyle changes and staying informed about emerging therapies offers the best strategy for effective blood sugar control and diabetes prevention.
nozaviral.com